Physician Burnout
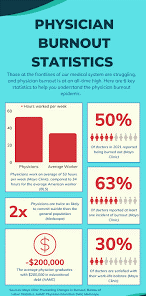
Physician burnout is a syndrome of chronic work-related stress that leads to emotional exhaustion, depersonalization (a cynical or detached attitude), and a low sense of personal accomplishment. It is a systemic issue, not a personal failing, driven by inefficiencies, administrative burdens, and increased technology requirements in the healthcare system.
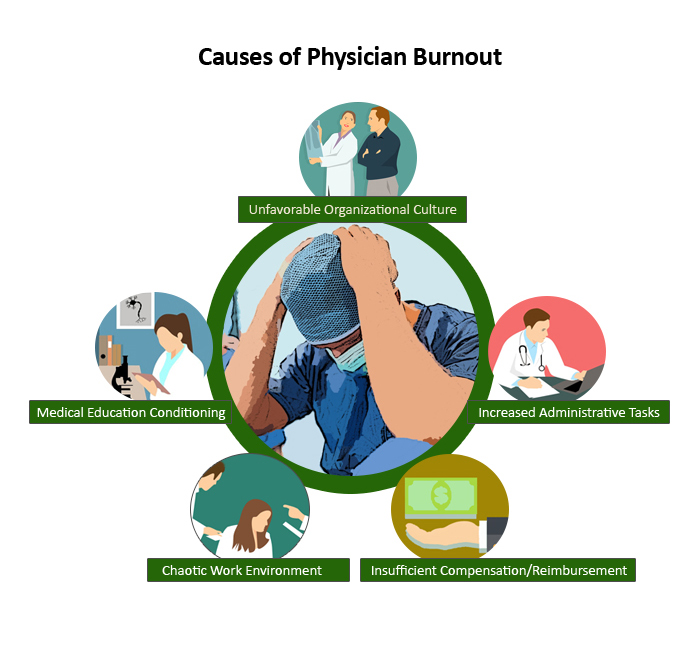

Causes
The primary drivers of physician burnout are systemic and environmental, stemming from the way modern healthcare is structured.
Excessive workload: This includes long hours, high patient volumes, and an unsustainable pace of work. Shortened patient visits and insufficient support staff also contribute.
Administrative burdens: Tasks such as complex electronic health record (EHR) documentation, insurance pre-authorizations, and other paperwork consume a significant portion of a physician’s day, pulling them away from patient care.
Lack of autonomy: Physicians are often constrained by administrative and bureaucratic constraints that limit their independence in clinical decision-making, leading to frustration.
Moral distress: Burnout is often tied to “moral injury,” a type of stress caused when physicians are forced to act in ways that conflict with their personal and professional ethics. This can include seeing patients suffer due to systemic problems like lack of resources.
Chaotic and fast-paced environments: Workplaces with high levels of chaos, interruptions, and time pressure contribute to burnout.
Erosion of meaning: Spending less time on fulfilling, meaningful patient interactions, and more on administrative tasks can deplete a physician’s sense of purpose.
Signs and symptoms
The symptoms of burnout extend beyond simple stress and can manifest both psychologically and physically.
Emotional exhaustion: Feeling drained, tired, and overwhelmed by the demands of the job.
Depersonalization (Cynicism): Developing a cynical or detached attitude toward one’s patients and work. This is sometimes called “compassion fatigue”.

Decreased personal accomplishment: Doubting your effectiveness and the value of your work.
Physical symptoms: Persistent fatigue, insomnia, anxiety, headaches, and gastrointestinal issues.
Behavioral changes: Increased irritability, withdrawing from colleagues, and losing interest in hobbies.
Consequences
The high rate of physician burnout has far-reaching consequences for physicians, patients, and the entire healthcare system.
Physician attrition: Burned-out physicians are more likely to reduce their work hours or leave the profession entirely, worsening healthcare access and physician shortages.
Mental health issues: Burnout is linked to higher rates of depression, anxiety, substance abuse, and increased risk of suicide among physicians.

Decreased quality of care: Burnout can impair a physician’s memory, attention, and executive function, which can lead to a higher risk of medical errors and adverse patient safety incidents.
Worse patient outcomes and satisfaction: Poor interactions with patients due to depersonalization can lead to lower patient satisfaction and trust, as well as poorer health outcomes.
Solutions and interventions
Effective solutions must address the systemic issues that cause burnout, not just individual coping mechanisms. The American Medical Association (AMA) and other organizations recommend:
System-level changes: Healthcare leaders should address root causes like workload, administrative burden, and inefficient EHR technology. Initiatives can include optimizing workflows, improving support staff, and providing more responsive tech support.
Promoting work-life balance: Organizations should provide more flexible scheduling and encourage the use of paid time off (PTO) without financial penalty.
Supporting professional fulfillment: Allow physicians to spend time (ideally at least 20%) on the aspects of their work they find most meaningful, such as education, research, or leadership.
Fostering a supportive culture: Cultivating a culture of wellness through peer-to-peer support, confidential mental health services, and mentorship can create a more supportive work environment.
Advocacy and policy change: The AMA advocates for policies, like removing stigmatizing questions about mental health from medical licensing applications, to make it easier for physicians to seek help